On October 10, US health officials said they had discovered a cluster of cases infected with a variant of the monkeypox virus (mpox) that is resistant to the antiviral drug tecovirimat (TPOXX) of Siga Technologies in five states of the country.
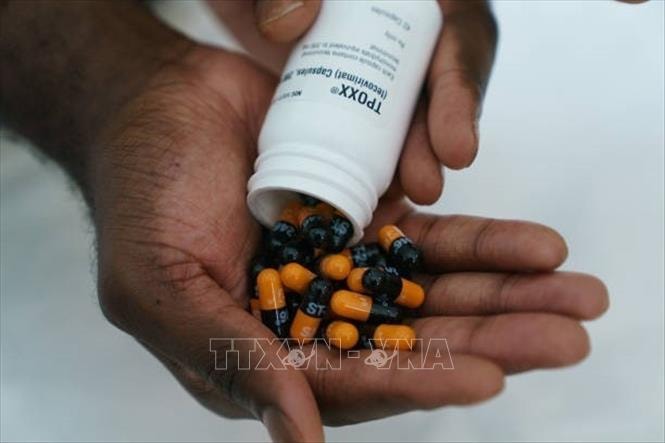
The US Centers for Disease Control and Prevention (CDC) reported that the drug-resistant cases involved a total of 18 individuals who contracted monkeypox caused by the Clade 2 virus between October 6, 2023, and February 15, 2024. All of these individuals had not received prior treatment.
Clade 2 infections, which are endemic to West Africa, caused a global outbreak of monkeypox in 2022 and continue to circulate at low levels in some countries. Health officials say new cases of Clade 2 infections may be underreported because not all monkeypox cases have been sequenced to identify the infectious variant. The report authors stress the need for regular surveillance to monitor for the emergence of resistance to maintain the effectiveness of TPOXX, one of the few drugs approved to treat monkeypox.
CDC officials also urged doctors to follow TPOXX's protocol closely, ensuring that patients take the drug correctly. The CDC said there is still a risk of spreading monkeypox while patients are taking the drug, so other methods of treating the dangerous disease are needed.
Previously, on August 14, the World Health Organization (WHO) declared monkeypox a global public health emergency (PHEIC), as the number of cases of the Clade 1b variant (which is more contagious and has a higher risk of death) skyrocketed in the Democratic Republic of Congo and spread beyond its borders. PHEIC is the WHO's highest level of warning for an epidemic.
Monkeypox typically causes flu-like symptoms and pus-filled sores. It is usually mild, but can be fatal or lead to serious complications in some cases, especially in children, pregnant women, and people with weakened immune systems, such as those with HIV.